The symptoms of prostatitis can make a man's life unbearable. Experienced doctors will help you quickly deal with the problem.
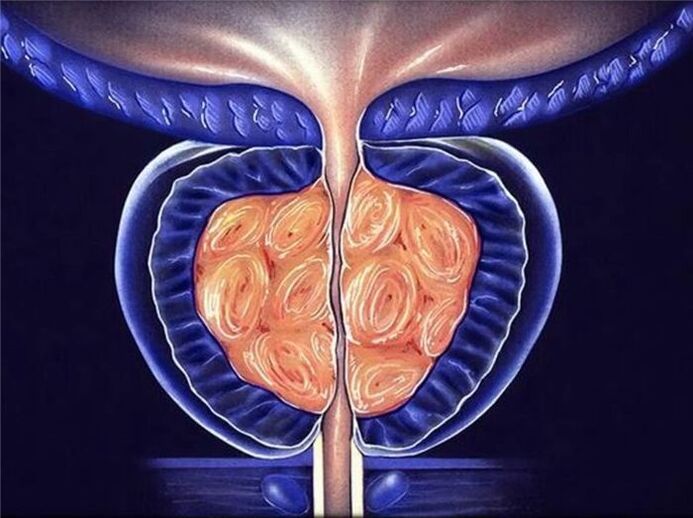
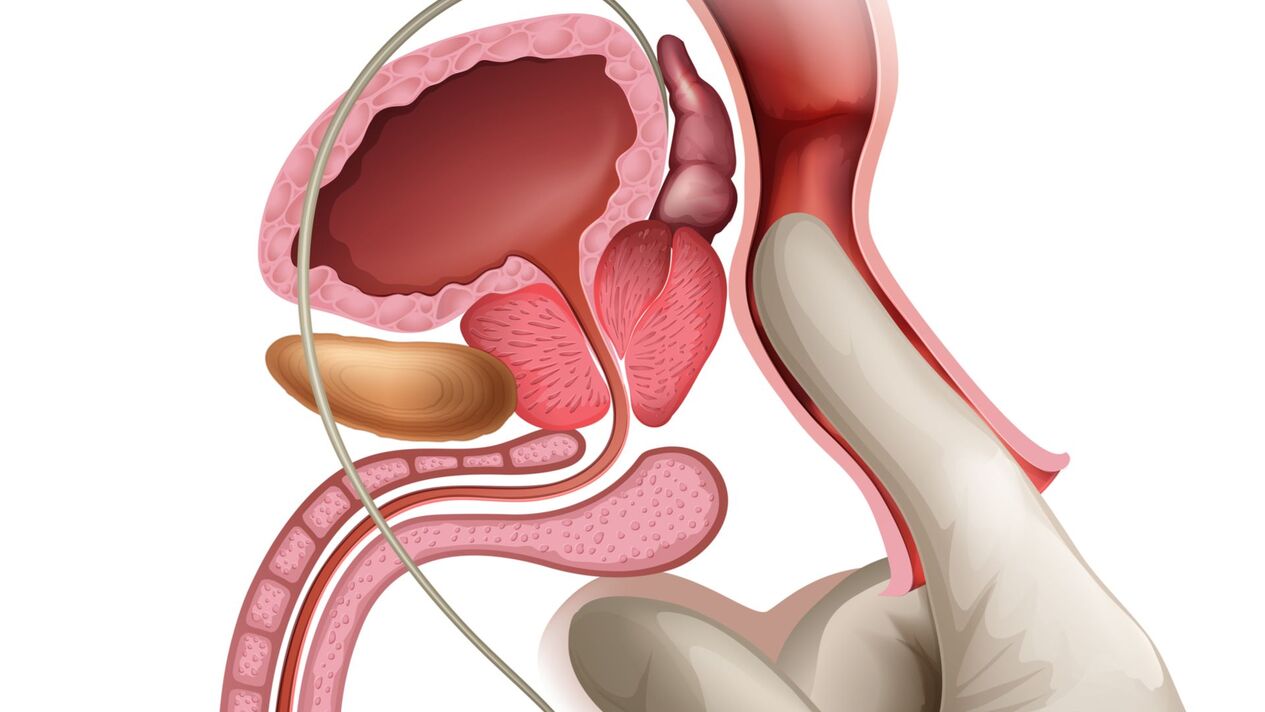
Inflammation of the tissues of the prostate gland (prostate) is called prostatitis. The prostate is an endocrine organ that affects several processes in the male genitourinary system. When it is inflamed, there is a violation of the urinary function, difficulties with potency, libido and ejaculation. Manifestations of prostatitis significantly worsen the quality of life, affect reproductive function. According to statistics, today inflammation of the prostate is the most common disease of the genitourinary system in men.
Signs of prostatitis
Symptoms of the disease can be both acute and almost invisible. If you find that you are experiencing the following symptoms, even if they are minor, it is better to immediately consult a doctor to confirm or refute the diagnosis.
- Micturition disorders: frequent urges, especially during night sleep, weak or intermittent flow, pain accompanied by difficulty urinating.
- Pain in the lower abdomen that radiates to the anus, scrotum, perineum.
- Decreased libido, impaired potency or sexual dysfunction.
- Change in consistency, color, quantity of ejaculate, difficulty ejaculating.
When identifying signs and symptoms of prostatitis in men, do not self-medicate or use recommendations from the Internet. At best, they will not help you, at worst - they can harm you. In addition, an untimely visit to the doctor provokes a worsening of the condition.

Signs of different types of prostatitis
According to the nature of the flow, there are:
Characteristic symptoms of acute prostatitis:
- fever, a sharp increase in body temperature (up to 40 degrees);
- severe headache, weakness, fatigue, irritability;
- pain in the groin, back, when urinating, frequent urges;
- change in the quality of urine (becomes cloudy, viscous, mixed with blood), unusual discharge from the urethral canal appears.
If you do not seek medical help in time, acute prostatitis can cause complications:
- abscess in the body of the prostate;
- vesiculitis (inflammation of the seminal vesicles);
- colliculitis (inflammation of the seminal tubercle);
- the appearance of scars and adhesions in the gland and spermatic cord;
- stagnant processes in the tissues of the prostate gland;
A feature of the chronic form is the blurring of the clinical manifestations and symptoms of prostatitis. The manifestations are similar to the acute form, but have a slow nature. The causes of the pathology, as a rule, are abacterial prostatitis, prostatosis (blood stagnation in the vessels).
Diagnosis and treatment
Inflammation of the prostate gland has a characteristic clinical picture. An experienced urologist can easily make a diagnosis after taking an anamnesis, examination and palpation, laboratory and instrumental studies (general and bacterial tests of urine and blood, blood tests for PSA, samples of prostate secretion, spermogram, ultrasound).

In the event that the patient turns to a specialist in time, the treatment of prostatitis includes an integrated approach and gives excellent results.
The modern clinic is equipped with modern high-tech equipment for diagnosis and treatment of diseases of the genitourinary system. Qualified delicate doctors will provide you with effective and most appropriate help.
Symptoms of prostatitis: pain, burning, discharge, pain, incontinence
The symptoms of prostatitis are most often of 3 types:
- urination disorder: difficult, frequent, nocturnal urination.
- pain symptoms: pain in the perineum, lower abdomen, groin. The pain may radiate to the scrotum or sacrum.
- mixed form, in which there are both urinary disorders and pain.
Causes of prostatitis?
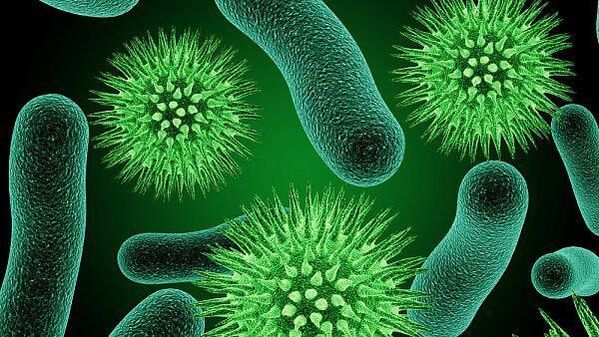
For bacterial prostatitis
The infection enters the prostate gland from neighboring organs: through blood and lymphatic vessels from a distant inflammatory focus (tonsillitis, sinusitis, caries).
The most common bacteria found in prostatitis are: Escherichia coli, Klebsiella, Proteus, Staphylococcus aureus, Enterococci.
The role of sexually transmitted infections: chlamydia, mycoplasma, trichomonas is discussed.
The activity and, accordingly, the manifestations of the inflammatory process depend on the properties of the microorganism, on the state of the pelvic organs, their blood circulation, concomitant diseases and other predisposing factors.
For non-bacterial prostatitis
Stagnation plays an important role. Disruption of blood flow causes swelling, exudation of prostate tissues and creates conditions for the development of an inflammatory process that is not related to a bacterial agent.
STDs and prostatitis
The question of the involvement of sexually transmitted infections in the development of prostatitis is widely discussed in scientific medical circles. There is no consensus on this matter.
We consider ourselves supporters of the direct connection between infections, the occurrence and course of prostatitis.
Why is prostatitis dangerous?
Prostatitis does not pose a threat to the patient's life, the process is chronic, worsening the quality of life.

Initial prostatitis. How to determine? First signs
The first signs of prostatitis are a change in the nature of urination: difficult, frequent urination, frequent urges to urinate, especially at night. Discomfort when urinating and pain of varying intensity in the groin.
Prostatitis age? Is this a disease of the young and/or the old?
Prostatitis is an inflammatory disease, so it can appear at any age. But adenoma or hyperplasia of the prostate is an age-related disease in men over 50 and is associated with the development of a benign prostate tumor.
Chronic prostatitis. Is it possible to cure it?
Having a diagnosis of chronic prostatitis implies the presence of changes in the structure of prostate tissues that remain for life. Like any chronic disease, prostatitis progresses through alternating periods of exacerbation and remission - a period when nothing bothers the patient. With proper treatment and lifestyle, periods of remission can be very long and complaints will never bother the patient again.

Bacterial and other types of prostatitis
There are various classifications, the most commonly used being developed by the US Institute of Health in 1995:
- Category IAcute prostatitis.
- II category.Chronic bacterial prostatitis.
- III category.Non-Bacterial Prostatitis/Chronic Pelvic Pain Syndrome - without obvious signs of infection and lasting 3 months or more.
- Subcategory III A.Chronic inflammatory pelvic pain syndrome (with leukocytes in prostatic secretion and pathogen release).
- Subcategory III B.Chronic non-inflammatory pelvic pain syndrome (no leukocytes in prostatic secretion).
- IV category.Asymptomatic prostatitis (with leukocytes in the prostate secretion, but without complaints).
For easier understanding, the classification can be represented by 3 types:
Acute prostatitis- occurs with severe pain, fever, impaired urination. In the secret of the prostate - a large number of leukocytes, which indicates a clear inflammatory process. It occurs, as a rule, for the first time in this patient. If these symptoms appear in a patient with chronic prostatitis, then they are called an exacerbation of chronic prostatitis.
Chronic bacterial prostatitis- Periodically, the patient's alarming symptoms, as a rule, are less pronounced than in acute prostatitis. When diagnosing, there is also an increase in leukocytes in the secretion of the prostate, it is possible to identify the cause of the inflammation.
The most difficult to diagnose isnon-bacterial prostatitis, or the so-calledchronic pelvic pain syndrome. This is due to the fact that the complaints are very similar to prostatitis, but are associated with diseases of other organs and systems, in which it is not possible to detect signs of inflammation and pathogenic bacteria: spasm of the pelvic muscles, impaired interaction between the muscles ofthe bladder and its sphincter, anatomical disorders - strictures (narrowing) of the urethra, leads to inflammation due to increased pressure inside the lobules of the prostate gland.
Who treats prostatitis - andrologist or urologist?
Prostatitis is treated by both a urologist and an andrologist.
An andrologist is a urologist who deals with diseases of the male genital and reproductive sphere.
Methods and schemes for the treatment of prostatitis
All prostate treatment regimens consist of drugs: drugs that improve the contraction of the prostate and bladder while relaxing the sphincter.
Good results are achieved with the simultaneous use of drugs and physiotherapy (massage of the prostate, complexes for the treatment of prostatitis).
What tests are given for prostatitis?
Fordiagnosis of prostatitisa consultation with a urologist (andrologist) is necessary to collect the patient's complaints, history, microscopy of prostate secretions and ultrasound diagnostics.
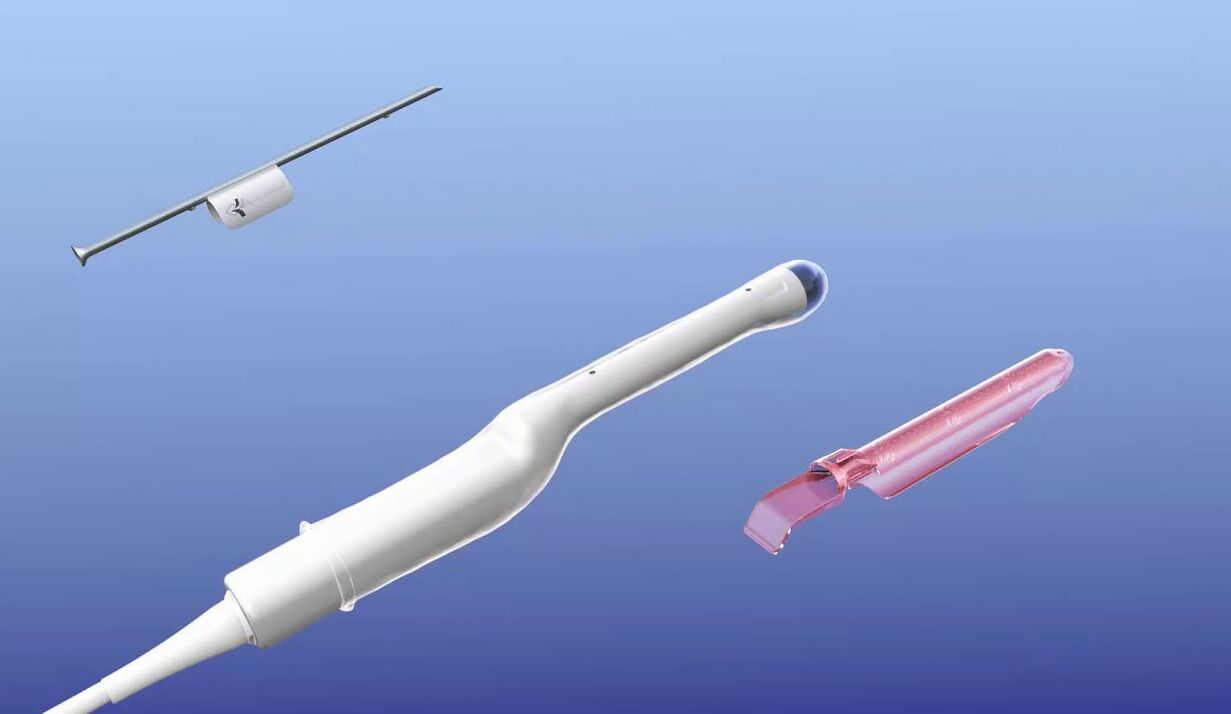
Transrectal ultrasound of the prostate (TRUS) and prostatic secretion obtained after prostate massage for microscopic examination are used for diagnosis.
In addition, seeding of the prostate gland secretion on the bacterial flora can be used to determine the sensitivity of the inoculated microflora to antibiotics.
Surgical interventions and operations for prostatitis
In prostatitis, operations are practically not used. With the exception of prostate abscess - a process in which foci with purulent contents are formed.
Can you cure prostatitis yourself?
In the presence of severe symptoms, it is better to be treated by a specialist, the time factor is of great importance in the treatment, because the longer the inflammation lasts, the greater the probability of irreversible changes in the organ.
But it is better to do prevention yourself, no doctor will do it for you.
Avoid hypothermia, overload from prolonged sitting, sexually transmitted infections, irregular sexual activity - all this is the way to effectively prevent prostatitis.
Medicines for prostatitis
Medicines for the treatment of prostatitis are divided into groups according to the mechanism of action:
Antibacterial agents (antibiotics)are prescribed only in the presence of a diagnosis: chronic bacterial prostatitis. The most commonly used are fluoroquinolones, macrolides and drugs from the doxycycline group.
Alpha blockers:are prescribed to restore impaired urination, increase the contraction of the bladder and relax its detrusor.
a large groupbiogenic stimulants and herbal preparations.
Effective treatment is possible only with a correct diagnosis, since there are no universal drugs for all types of prostatitis. Often, patients take drugs to treat prostatitis if they have a completely different disease, but with similar symptoms.

Nuts, roots, parsley, cucumber, honey, bees, leeches and other folk remedies for prostatitis
Folk methods of treatment have the right to exist, but you should understand that it is very difficult to choose a folk method that suits you. On request, treatment of prostatitis with folk methods, the search engine gives 70 million results.
Folk methods have not been tested for effectiveness. What helped one patient with such treatment (and whether it helped) does not at all mean that it will help you.
Exacerbation of prostatitis after treatment. remission, relapse
All chronic inflammatory processes have periods of exacerbation and remission, when nothing bothers the patient. The duration of remission can be different and depends on many factors, including whether the patient is undergoing prophylactic treatment. Patients who periodically carry out prophylactic treatment without waiting for a deterioration in well-being, as a rule, have less frequent exacerbations.

Prostate massage at home. Is massage always necessary for prostatitis?
Prostate massage can also be done at home if you are married to a urology nurse. Each medical manipulation has its subtleties and nuances. Only a doctor can determine the indications for this procedure, so in some diseases: prostate adenoma (in the presence of acute urinary retention) prostate massage is not desirable, and in tumors it is contraindicated.

alcohol and prostatitis
Alcohol itself does not cause the development of prostatitis, but it is a factor that increases the stagnation and swelling of the prostate gland and thus contributes to its development.
Sex life and prostatitis
There is a direct relationship between the intensity of sexual activity and prostate disease. With prolonged abstinence, stagnation occurs in the prostate, which worsens metabolic processes and disrupts blood microcirculation, which contributes to the development of inflammatory processes. Regularity is more important to prostate health than intensity of intercourse. Excessive sexual contact, especially with different partners and unprotected from infection, is the fastest way to prostatitis.

Does prostatitis affect women?
The impact on the health of a woman with prostatitis in her partner is, of course, there. The prostate, together with the seminal vesicles, produce the liquid component of the semen, which during sexual intercourse enters the partner's genital tract. The main danger can be the presence of a sexually transmitted infection or bacterial prostatitis, which can provoke inflammatory diseases in women.
Pregnancy and prostatitis
Since the prostate gland produces the liquid part of the semen, which contains nutrients for the sperm, often with prostatitis there is a decrease in the quality of the sperm, making it difficult to get pregnant.
Prevention. What to do to avoid prostatitis?
Prevention is directly related to the climate in which the patient lives and his profession.
Prevention of prostatitis is to avoid and minimize the factors that contribute to the development of prostatitis. It is necessary to avoid hypothermia, to alternate sedentary work with periods of physical activity. Regular sex life is important for prostatitis.
The prostate. What it is and how its health affects a man's fertility

A diseased prostate is often the cause of many unpleasant diseases, it can make sexual intercourse difficult for a man and even disrupt his fertility. Not to mention that every year in every European country tens of thousands of men get prostate cancer.
Many men are ashamed of their prostate problems and do not go to a urologist. Learn more about the prostate itself, its diseases, and its connection to infertility in this article.
What is the prostate for?
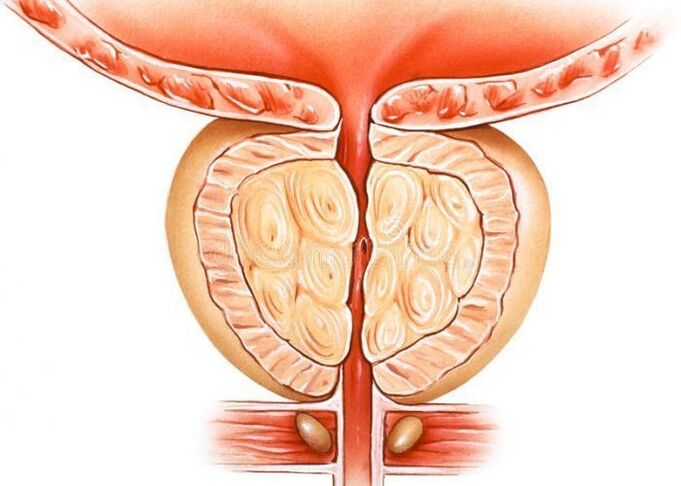
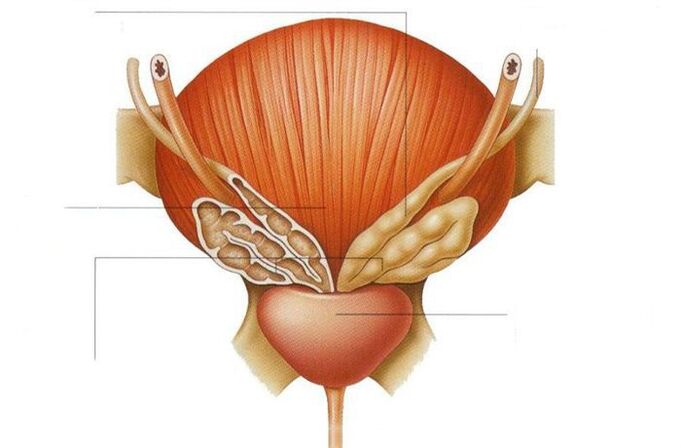
The prostate, also known as the prostate gland, is modest in size, about the size of a walnut, but it has a very important reproductive function. The gland is located at the intersection of the urinary tract - under the bladder, right at the mouth of the urethra, which also passes right through the center of the organ.
The prostate is a gland, that is, just as the sweat glands secrete sweat and the liver secretes bile, the prostate secretes a substance that performs a specific function in the body. This substance is a cloudy whitish liquid in semen. In other words, the secretion produced by the prostate is part of the sperm and fulfills the function of nutrition. Thanks to it, the sperm can maintain the necessary parameters - to be quite viable and mobile.
In addition, the prostate gland produces the protein substance PSA, which is involved in the fertilization process. Thus, there is no doubt that male fertility largely depends on the state of the prostate, and any problems with the prostate gland can make it difficult to conceive a child, as they are associated with a decrease in sperm parameters.
Prostate size changes throughout life
A boy is born with a prostate the size of a pea. Over the following years, the gland slowly enlarges to reach the correct size for an adult male around the age of 30. A man's prostate "in its prime" is about 2. 5cm high, 4cm wide and 3cm thick and weighs between 15 and 20g.
30 years is a period of relative stabilization, during which the prostate does not grow as fast as before. It increases again around age 45. This is due to a decrease in the level of male sex hormones, including the most important of them - testosterone.
When the size of the prostate changes, we are talking about the so-called benign prostatic hyperplasia, which even at this stage can be associated with unpleasant symptoms.
Benign prostatic hyperplasia - what are the symptoms?
The most common symptoms that men with benign prostatic hyperplasia complain of are:
A person may also feel that their bladder is not completely empty. In addition, urine may leak out of the bladder in an uncontrolled manner.
All these symptoms are the result of the pressure of the enlarged prostate on the urethra, making it difficult for urine to drain properly. Stagnation of urine in the bladder, in turn, can cause recurrent urethral infections, bladder infections and stone formation, and in the worst case, even kidney failure.
But the worst thing is that similar signs accompany other dangerous pathologies - prostatitis and prostate cancer. That is why it is so important that a person contacts a urologist as soon as he notices the first alarming symptoms.
Acute and chronic prostatitis mainly affects young men
Prostatitis can be bacterial or non-bacterial in origin. It can be caused by germs or stagnation of secretion produced by the prostate gland. It mainly affects young men between the ages of 20 and 40.
- increased urge to urinate;
- burning sensation when urinating;
- sometimes an increase in body temperature.
Treatment of prostatitis is not the easiest, since many antibiotics do not penetrate well into the prostate gland.
Prostatitis is one of the main causes of male infertility. Treatment of this pathology is strictly necessary.
Prostate cancer is another disease of the prostate.
In Europe, prostate cancer is one of the most common cancers in men. Every year, in every country, doctors diagnose it in tens of thousands of people. According to statistics, this cancer affects approximately 30% of 50-year-old men and 80% of 80-year-old men. At the same time, it is the third leading cause of death from cancer.
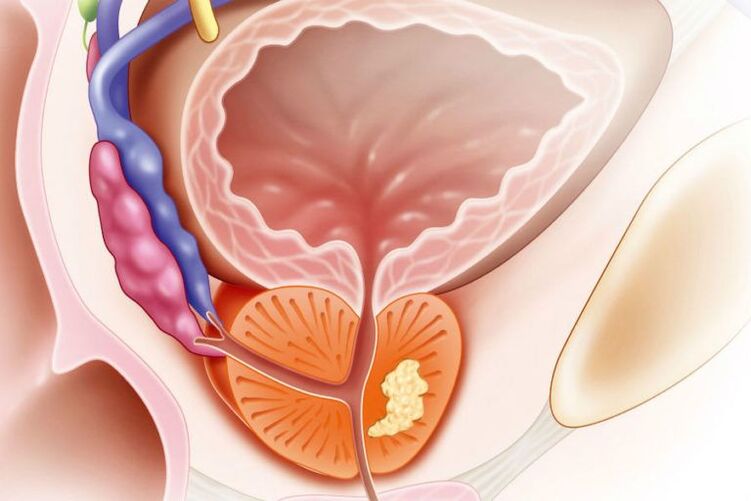
Prostate cancer
A characteristic feature of prostate cancer is that it develops quite slowly and is usually asymptomatic - at least in the beginning. If symptoms are present, they are very similar to those associated with benign prostatic hyperplasia.
Are there men at increased risk of developing this cancer? yesPredisposition to prostate cancer will be obesity and a sedentary lifestyle, untreated inflammation of the urinary tract, excessive sexual abstinence, as well as genetic factors.
Prostate cancer is curable if detected early. Unfortunately, many men postpone visiting a urologist most often due to shame and fear of a painful and unpleasant diagnosis. In the meantime, it is enough to pass a few simple tests to protect yourself from this dangerous disease.
As for fertility, with advanced prostate cancer, infertility is guaranteed. That is why a timely examination by a urologist is the key to a man's reproductive health.
prostate massage
Prostate massage is a useful urological manipulation aimed at maintaining men's health. It helps restore blood supply to the pelvic organs, normalize metabolic processes, improve tissue regeneration, increase the effectiveness of drug treatment, drain accumulated toxins and pus residues, increase the body's immune resistance and solve potency problems.
In a specialized medical clinic, you can take a course of therapeutic prostate massage to eliminate unpleasant symptoms or restore potency at a convenient price. The procedure is performed by urologists with the highest qualification category. The rich experience of the specialists allows us to perform a delicate procedure with minimal discomfort for the patients. The price of the massage is calculated individually depending on the condition of the patient.
Purpose of therapeutic prostate massage
Therapeutic massage is an effective prevention of the development of various diseases of the prostate gland (including cancer). It promotes the outflow of prostate secretion, reduces inflammation, improves muscle tone.
The procedure helps to get rid of discomfort and pain in the perineum, and also increases sexual activity and potency. It is usually combined with drug therapy, making it more effective.
The price of prostate massage depends on the duration of the course, which is selected individually by a professional urologist of the medical center, depending on the patient's condition.
If you want to make an appointment with a specialist or specify the price of the service, use the feedback form or call the 24/7 phone number listed on the site. Our consultants are always ready to answer all questions in as much detail as possible.
Indications for prostate massage
The main indication for therapeutic massage of the prostate is diagnosed prostatitis of infectious or non-infectious origin. It is also prescribed for:
- chronic pelvic pain;
- congestion in the prostate;
- hereditary predisposition to prostatitis;
- erectile dysfunction caused by pathologies of the prostate gland;
- decrease in male sexual activity.
The effectiveness of prostate massage for these problems has been confirmed by numerous clinical studies. Our patients tolerate the manipulation very well, as it lasts 1-2 minutes and is maximally painless. The doctor always controls the force of pressure on the prostate gland, depending on the individual feelings of the man.
How is a prostate massage performed?
Results of the procedure:leakage of prostatic secretion
The patient assumes a knee-elbow position or lies on his side. The doctor puts on gloves and inserts a finger into the rectum to a depth of 4-5 cm. Then he gently massages the prostate until the secret begins to stand out from it.
In case of chronic prostatitis, the doctor will prescribe a course of prostate massage. As a rule, it includes from 10 to 15 procedures, carried out at an interval of 2-3 days. After completing the course, there is a break for 2-3 weeks, after which the procedures are repeated.
Useful information
In some cases, exposure to the prostate is undesirable. The manipulation is not performed in case of acute bacterial prostatitis and other infections of the genitourinary system, in case of stones, abscesses, malignant tumors of the prostate, hemorrhoids, urinary retention.























